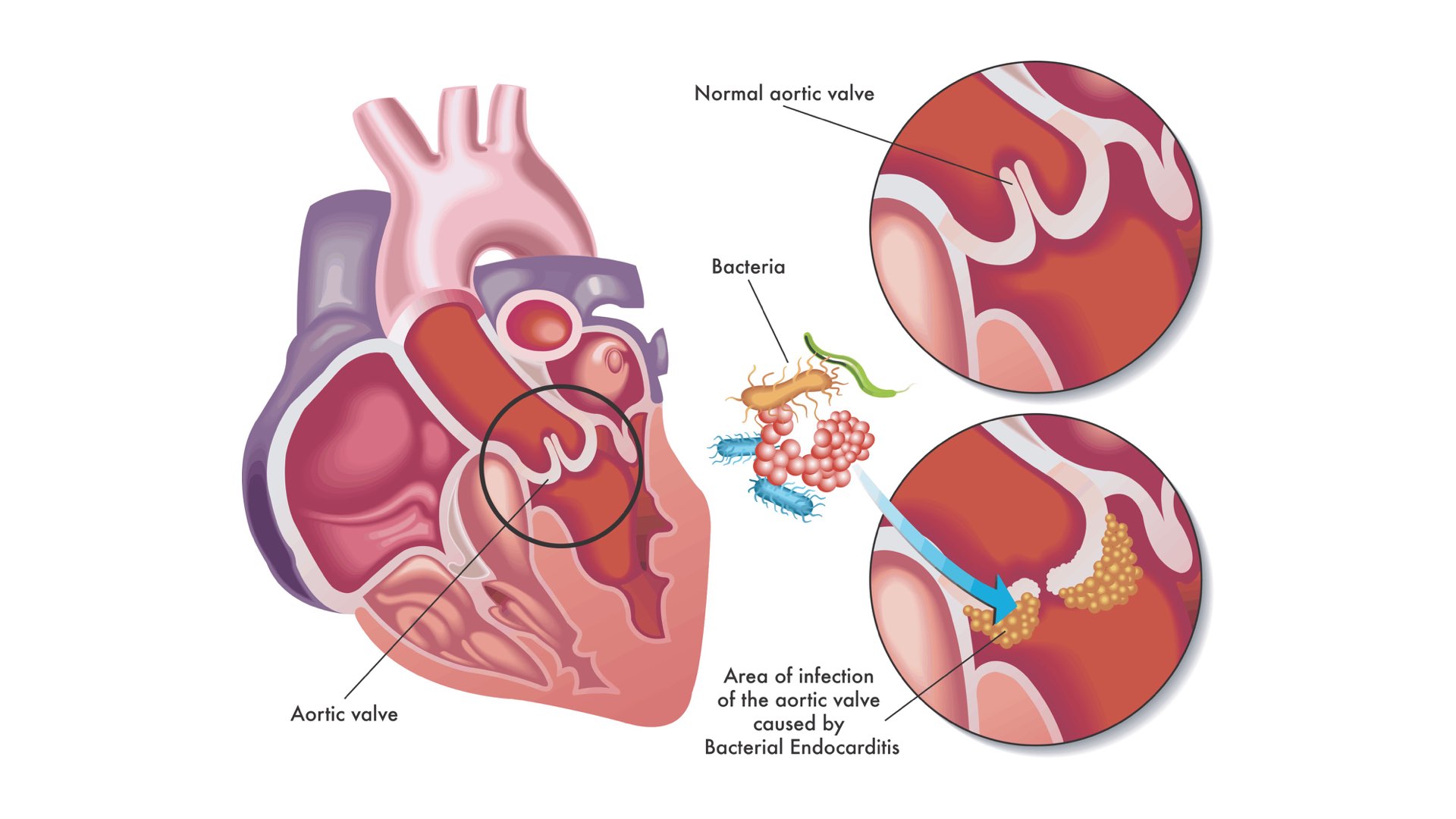
If you have a heart condition, you may have heard about infective endocarditis. Infective endocarditis is a condition where the lining of your heart, and sometimes the heart valves, become infected. It is a very serious condition and can be fatal. It is most commonly caused by bacteria entering the blood stream and travelling to the heart. It is a rare condition; the risk of infective endocarditis in the general population is less than 1 case per 10,000 people a year.
Some people, with a cardiac condition, are at a higher risk. This includes;
- Some diseases that affect the heart valves
- Having a prosthetic/replacement heart valve
- A condition called hypertrophic cardiomyopathy;
- If you have previously had infective endocarditis, you are more at risk of getting it again
- Congenital heart disease – this is a general term for a range of birth defects that affect the normal way the heart works.
Certain dental treatment can pose a very small risk of developing infective endocarditis.
The mouth is full of bacteria, and if your dentist provides some treatment where you experience some bleeding, such as having a tooth removed, the bacteria from your mouth may be more likely to enter the blood stream and travel to the heart.
Everyday activities, such as brushing your teeth or flossing can also cause your gums to bleed and create a way bacteria can enter your blood steam, though again the risk is very low. Because of this it is really important to maintain good oral hygiene to reduce the risk from bacteria in your mouth.
Before 2008, the recommended practice was for dentists to arrange for patients with pre-disposing heart conditions to take a dose of antibiotics prior to their dental treatment to try and prevent infective endocarditis. This is called antibiotic prophylaxis.
In 2008, after reviewing the evidence, a new set of guidance came out that antibiotic prophylaxsis was not recommended prior to dental treatment.
Confusing right?
Fortunately, in 2018 the Scottish Dental Clinical Effectiveness Programme, which helps develop evidence based guidance for dentists to follow, released some new guidance that aimed to help clarify this matter. This guidance was endorsed by the The Faculty of General Dental Practice UK (FGDP(UK)) and the National Institute of Clinical Effectiveness (NICE), so it is pretty much the go-to guide for dental care professionals in the UK.
Firstly, it clarifies why dentists don’t normally prescribe antibiotic prophylaxis:
- Dental procedures are no longer thought to be the main cause of infective endocarditis.
- It is unclear whether antibiotic prophylaxis prevents infective endocarditis and therefore it may occur whether or not prophylaxis is given.
- Antibiotics can cause side effects, such as nausea, diarrhoea and allergic reactions and, in rare cases, anaphylaxis (a life threatening allergic reaction).
- Antibiotic resistance is on the rise due to the antibiotics being prescribed when they aren’t needed. This means certain infections are becoming more difficult to treat because antibiotics are less effective against these resistant strains of bacteria.
Following on from this, the guidance states that most people at increased risk of infective endocarditis don’t need antibiotics before they have dental treatment.
However, some patients (for example if they have a condition from the list above) may need to be further assessed. If this is the case your dentist will ask for your consent to write to other health care professionals involved in your care, such as your cardiologist, asking for their opinions on whether they think antibiotics should be recommended. They will then discuss with you the risks and benefits of having antibiotics prior to dental treatment, so you can make an informed decision on whether having antibiotic prophylaxis is right for you.
If you are at increased risk of infective endocarditis, following your dental treatment your dentist will advise you to see your GP if you develop any of the following:
- A high temperature (fever) of 38 degrees C or above
- Sweats or chills, especially at night
- Breathlessness, especially during physical activity
- Weight loss
- Tiredness (fatigue)
- Muscle, joint or back pain (unrelated to recent physical activity)
Although these are more likely to be symptoms of a much less serious infection, they can be early signs of infective endocarditis and require investigation. Make sure to tell your GP if you’ve had any recent dental treatment.
Finally, the guidance provides a list of the best ways of reducing your risk of developing infective endocarditis, which your dentist will discuss with you:
- Look after your oral health – clean your teeth regularly and carefully using fluoride toothpaste. Good oral hygiene will not only reduce your risk of developing dental disease, it will also reduce the chance of bacteria entering your blood stream.
- Be sure to attend regular dental check-ups so that any dental disease is treated before invasive dental treatment is needed.
- Cut down on sugary snacks and drinks to reduce your chance of developing dental disease.
- Do not smoke as smoking is a major risk factor in dental disease such as gum disease.
- Cut down the amount of alcohol that you drink. Again this reduces your chance of developing dental disease as well as being good for your general health.
- The guidance also recommends looking after your skin as a break in the skin is another way that bacteria can enter your blood. The guidance recommends you regularly wash your skin with soap and water and wash any cuts or grazes carefully to prevent them becoming infected.
- Avoid non-medical procedures that involve piercing the skin, including body piercing or tattooing.
If you have any questions about infective endocarditis, speak to your dentist.
Alternatively, there are lots of resources and information available. The SDCEP guidance, which I reference in this article, offers a video introduction to the guidance and patient advice leaflets. It also has the full guidance which shows how these recommendations were made, and what evidence was reviewed to make it.
Keep updated with the Online Dentist newslettersign up today
Recent Articles
 Tooth decay is when you get holes (also known as cavities) in your teeth. This is caused by bacteria in plaque. It’s one of the main reasons why you need...
Tooth decay is when you get holes (also known as cavities) in your teeth. This is caused by bacteria in plaque. It’s one of the main reasons why you need...
 NB: If you come to this section in a rush because someone has knocked an adult tooth completely out, go to ‘Knocked out adult tooth’ article. Of course young children...
NB: If you come to this section in a rush because someone has knocked an adult tooth completely out, go to ‘Knocked out adult tooth’ article. Of course young children...